What is follicle stimulating hormone (FSH)?
FSH is a hormone that stimulates tube-like structures in the ovaries, called follicles, to grow.
What is Clomid?
What is Clomid fertility medicine? This drug triggers the levels of two follicle-promoting hormones to increase in the body: follicle stimulating hormone (FSH) and luteinizing hormone (LH).
What is luteinizing hormone (LH)?
In women, LH helps activate egg production. In men, LH triggers an increase in the levels of testosterone, a hormone which stimulates sperm production.
What is follicular phase?
During the first half of a woman’s menstrual cycle, three things happen: the uterus thickens, eggs mature inside the follicles, and estrogen levels increase. Collectively, this stage is called the follicular phase.
What is gamete intra fallopian transfer (GIFT)?
A medical procedure in which a surgeon removes eggs, mixes them with sperm, and inserts them back into the woman’s fallopian tubes. In GIFT, fertilization happens inside the woman’s fallopian tubes.
What is intra uterine insemination (IUI)?
IUI is a fertility treatment in which a surgeon places sperm directly next to the cervix inside the vagina (cervical cap insemination). People often take ovulation medicines to help improve the chances of pregnancy when doing IUI. This fertility treatment can be performed with donor sperm or with a partner's sperm: (IUI) with donor sperm (donor insemination), IUI with husband or partner sperm (Husband IUI or Partner IUI).
What is Fertility Treatment?
The collective procedures couples undergo to treat their infertility. Common types of fertility treatments include in-vitro-fertilization (IVF).
What is artificial insemination?
Artificial insemination is a term which is being replaced by more specific terms such as intrauterine insemination (IUI) with donor sperm (donor insemination), IUI with husband or partner sperm (Husband IUI or Partner IUI) or fertility treatment in which a surgeon places sperm directly next to the cervix inside the vagina (cervical cap insemination). People often take ovulation medicines to help improve the chances of pregnancy when doing IUI.
What is azoospermia?
A medical condition in which a man has no detectable levels of sperm. Low sperm production or blockages of a reproductive tract can common causes.
What is basal body temperature (BBT)?
BBT is your lowest body temperature within a 24 hour time-frame. Since your BBT alters according to your ovulation cycle, it can help predict time of ovulation. Usually, your BBT slightly increases when your follicles start to release eggs (ovulation). Tracking your BBT using a chart is a useful way to predict time of ovulation and create an ovulation calendar.
What is cervical mucus?
A sticky fluid covering the cervix. It changes in consistency throughout a woman’s menstrual cycle. During ovulation, the cervical mucus becomes more watery and stringy so sperm can pass through more easily.
What is an ectopic pregnancy?
An ectopic pregnancy happens when an embryo implants anywhere outside of the uterus. It usually occurs inside the fallopian tube.
What is Fertility?
The quality or state of being fertile - the ability to get pregnant through sexual intercourse within one year
What is Infertility?
A of the reproductive system condition defined by the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse.
What is Fertility Care?
Interventions that include fertility awareness, support and fertility management with an intention to assist individuals and couples to realize their desires associated with reproduction and/or to build a family.
What are Fertility Clinics?
Medical clinics that help women and men who want to become parents but for medical or other reasons have been unable to achieve this goal via the natural course.
Who are Fertility Physicians?
The physicians who work with couples undergoing fertility treatments. ARC’s network physicians are board-certified reproductive endocrinology and fertility specialists and also board-certified obstetrician/gynecologists.
What is hCG (Human Chorionic Gonadotropin)?
hCG is the pregnancy hormone made by the placenta that stimulates the ovaries to make estrogen and progesterone which thicken your uterine lining and tell your body to stop menstruating (or releasing eggs). hCG increases until about 10 weeks of pregnancy. hCG is the hormone that is used to detect early pregnancy. hCG can also be injected at mid-cycle in ovarian stimulation cycles and IVF cycles to stimulate ovulation.
What is Hysterosalpingogram (HSG)?
A radiology procedure that examines the health of the uterus and fallopian tubes. A radio-opaque fluid is injected into the uterus and fallopian tubes and photographed via x-rays to check the shape of the uterus and tubes, and whether they contain any infections or injuries (such as fibroids, or scar tissue).
What is in-vitro fertilization (IVF)?
A fertility treatment in which a surgeon removes eggs from a woman and injects concentrated sperm into the eggs inside a petri dish. The entire procedure happens outside of the body. After the eggs are successfully fertilized, the surgeon transfers the embryo back into the woman’s uterus.
What is intra-cytoplasmic sperm injection (ICSI)?
A form of IVF which involves injecting a single sperm directly into a mature egg. A surgeon then transfers the fertilized egg into the woman’s womb.
What is anovulation?
A disorder in which there is an absence of ovulation. Anovulation can be caused by problems in the hypothalamus at the base of the brain, the pituitary gland, the ovaries, other hormone producing organs, or general health problems such as obesity.
What are Assisted Reproductive Technologies (ART)?
All interventions that include the handling outside of the body of both human eggs and sperm or of embryos for the purpose of reproduction. Thus, ART does not include intrauterine insemination (IUI) because eggs are not handled outside the body. Non-ART fertility treatments are covered under the term Medically Assisted Reproduction (MAR).
.
What is clomiphene citrate?
A common ovulation medicine available under several commercial names such as Clomid and Serophene.
What is a Corpus Luteum?
A glandular structure that forms after the follicle releases the egg (ovulation). The corpus luteum releases progesterone in the second half of the menstrual cycle. Progesterone helps prepare the uterus lining (the endometrium) for embryo implantation.
What is Dysmenorrhea?
Abnormal pain during menstruation.
What is Dypareunia?
Pain that occurs during sexual intercourse.
What is Egg Retrieval?
A surgical procedure done during fertility treatments, in which eggs are extracted from follicles. The specialist passes a small needle through the top of the vagina into the follicles. The eggs are then removed and placed into a test tube. An embryologist then looks for eggs under a microscope.
What is an Embryo Transfer?
The process of placing fertilized eggs (embryos) back into the woman’s uterus. The embryo transfer is painless and requires no anesthesia.
What is an Endometrial Biopsy?
A procedure in which a small sample of the uterine lining is removed and sent to a laboratory for evaluation. It is now rarely used.
What is Endometriosis?
A condition in which uterus lining cells grow outside the uterus causing inflammation, pain, adhesions, infertility and other pelvic problems.
What is Estradiol?
A female hormone produced by the ovary. Estradiol stimulates the endometrium (lining of the uterus) and is important in ovulation, pregnancy and other aspects of female health.
What is a Fibroid?
A fibroid is a benign tumor of the uterine muscle. It is also called a myoma.
What is Laparoscopy?
A minimally invasive surgical procedure that examines pelvic organs through a small telescope (laparoscope).
What is Luteal Phase?
The second half of the woman’s menstrual cycle (post-ovulation), marked by elevated progesterone levels..
What is Male Infertility?
Male infertility occurs when men have a less than normal semen analysis or other reproductive problem that reduces their chances of getting their partner pregnant. About 50% of infertility cases are reported to be associated with male infertility.
What is an Ovarian Cyst?
A fluid filled sac in the ovaries. Temporary cysts are related to hormonal abnormalities often associated with ovulation disorders. They almost always resolve on their own. Benign ovarian cysts are not caused by hormone abnormalities but by the growth of new tissue. The vast majority of these cysts are benign.
What is Ovarian Hyperstimulation Syndrome (OHSS)?
A condition that results from over stimulation of the ovary during ovarian (OS) .About 10% to 20% of women experience mild OHSS because the ovaries are enlarged, causing them to be painful and sensitive to pressure. There are many different ways to manage OHSS: reducing the dose of gonadotropin stimulation, bed rest, cancellation of the in-vitro-fertilization (IVF) cycle or the embryo transfer. Severe OHSS occurs in less than 1% of women undergoing OS and may require hospitalization.
What is Polycystic Ovarian Syndrome (PCOS)?
A disease diagnosed by at least two or three of the following conditions: 1) irregular or complete absence of ovulation 2) excess androgen levels in blood or increased hair growth 3) 24 follicles in both ovaries. Often associated with infertility and other medical problems.
What is a Post Coital Test (PCT)?
What is a Post Coital Test? This is a test that was once thought to predict pregnancy rates. This Post Coital Test procedure is no longer performed. It involves collection of cervical mucus from the cervix within a couple of hours after a woman has had intercourse. The mucus is then analyzed to look moving sperm.
What is Progesterone?
A hormone produced mainly during the second half of the menstrual cycle to stimulate uterine lining growth so the embryo can implant.
Who is a Reproductive Endocrinologist (RE)?
A physician specializing in obstetrics and gynecology (OB-GYN) with 3 years of additional training in endocrinology and infertility, a published thesis, two years of clinical practice and has passed rigorous written and oral examinations. Some obstetrician/gynecologists call themselves fertility specialists, but only those who meet strict requirements are Reproductive Endocrinologists.
What is a Resistant Ovary?
Ovaries that have a low or no response to ovarian stimulation with gonadotropins follicle stimulation hormone (FSH) and/or lutenizing hormone (LH).
What is a Semen Analysis?
A test that analyses sperm quality by evaluating ejaculate volume, appearance, consistency, sperm shape, sperm motility, sperm concentration and presence of certain antibodies.
What is Sperm Morphology?
The shape of ejaculated sperm. Strict morphology involves the use of very rigorous criteria for normal sperm shape.
What is Spermatogenesis?
The process of sperm production.
What is Testicular Biopsy?
A minor surgical procedure typically performed by an urologist to determine cause of testicular problems.
What is a Vasectomy?
A surgical procedure to occlude the vas deferens, the structure that transports sperm from the testicle to the end of the penis. Performed for male sterilization.
What is Zygote Intra-Fallopian Transfer (ZIFT)?
A procedure in which eggs are retrieved from a woman’s uterus and then fertilized in a specialized laboratory. The fertilized eggs are placed back into the fallopian tubes the day after. ZIFT is now rarely performed.
IVF Success Rates and Age: Understanding the Key Factors

Know the Facts and Maximize Your Chances of a Successful Birth at Any Age
In vitro fertilization (IVF) is a widely used assisted reproductive technology (ART) that has helped tens of millions of people realize their dreams of parenthood. IVF is a fertility treatment where eggs are retrieved from a woman's ovaries, fertilized with sperm in a laboratory, and then transferred back into the uterus where the embryo implants and develops into a baby. However, it is essential to understand that the success of IVF can be influenced by various factors, with age being one of the most significant. People looking to grow their family are faced with conflicting information about how to maximize their fertility, especially when it comes to aging. Information can range from depressingly negative to unbelievably optimistic, and it is difficult to find the truth of what aging means for fertility. It is important to understand the true correlation between IVF success rates and age, and for families considering this fertility treatment option to have the most accurate insights available.
Age and Fertility
Age is a crucial factor that significantly affects the success rates of IVF. The age of parents of any gender involved in the IVF process can impact the chances of success. However, the woman's age has a more pronounced effect due to the more rapid decline in fertility in women than men that occurs with age.
Diminished Ovarian Reserve
Diminished ovarian reserve is a condition in which a woman's ovaries have a reduced number of eggs. Diminished ovarian reserve is common in older women, resulting in fewer eggs available for fertilization during an IVF cycle. It is also important to note how egg quality (as measured by the number of eggs with normal chromosomes) also "declines significantly with age." This can lead to failed fertilization, failed implantation, miscarriage, or genetic disorders in babies.
Ovarian Stimulation and Age
Ovarian stimulation plays a vital role in IVF treatments by using hormonal medications to induce the ovaries to produce multiple mature eggs. Its primary objective is to enhance the likelihood of obtaining a sufficient number of eggs for fertilization during an IVF cycle. However, in older women, the response to ovarian stimulation can be diminished, resulting in a reduced number of eggs available for retrieval and subsequent fertilization.
Pregnancy Rates and Live Birth Rates
In terms of pregnancy rates and live birth rates, younger women generally have higher success rates with IVF compared to older women. Factors such as decreased egg quality, decreased implantation rates, and higher rates of miscarriage contribute to the decreased chances of getting pregnant through IVF as women age. Even with successful fertilization and implantation, the risk of pregnancy loss or chromosomal abnormalities increases with age.
Chronological Age vs Biological Age
While chronological age simply represents the number of years a woman has lived, biological age describes the condition and functionality of the woman’s health overall, including her reproductive system, which can be influenced by genetic factors, lifestyle choices, and overall health.
In the context of fertility and reproductive health, biological age and chronological age may not always align. Biological age is more important than the number of years a woman has lived when predicting the success of fertility treatments.
For example, a woman who is 40 years old chronologically may have a reproductive system that functions similarly to that of a woman in her early 30s, indicating a younger biological age. On the other hand, another woman who is 35 years old chronologically may have a reproductive system that exhibits characteristics associated with older age, indicating an older biological age.
Assessing biological age involves evaluating various factors, including:
- Ovarian reserve
- Hormone levels
- Reproductive organ health
- And other relevant markers of reproductive function
This assessment helps fertility specialists determine a woman's likelihood of success with fertility treatments, such as IVF, and develop personalized treatment plans tailored to her specific needs.
IVF Success Rates by Age
IVF success rates can vary significantly based on a woman's age. Generally, women under 35 have higher success rates compared to older women. As women age, their fertility declines, resulting in decreased egg quality, lower implantation rates, and higher rates of miscarriage. Therefore, older women, particularly those over the age of 35 or 40, may experience lower success rates with IVF due to age-related factors impacting both egg quality and quantity. It is important for women to understand the potential impact of age on IVF success rates when considering fertility treatments.
The average percentages of live births from IVF as reported by
The Society for Assisted Reproductive Technology for 2020 are:
| Women aged 35-37: | 30.7 % success rate |
| Women aged 38-40: | 21.3 % success rate |
| Women aged 40-42: | 11.3 % success rate |
| Women over the age of 42: | 3.6 % success rate |
Live births per intended egg retrieval
(All Embryo Transfers from One Egg Retrieval)
| Women under the age of 35: | 54.5 % success rate |
| Women aged 35-37: | 39.8 % success rate |
| Women aged 38-40: | 26.1 % success rate |
| Women aged 40-42: | 13.3 % success rate |
| Women over the age of 42: | 4.0 % success rate |
Statistics for All Embryo Transfers For a New Patient
Another way to look at success rates by age is the number of live births per new patient. This includes many women who did more than one egg retrieval. SART reports these as follows:
| Women under the age of 35: | 68.9 % success rate |
| Women aged 35-37: | 58.2 % success rate |
| Women aged 38-40: | 43.0 % success rate |
| Women aged 40-42: | 23.6 % success rate |
| Women over the age of 42: | 7.0 % success rate |
These statistics provide an overview of average success rates and should not be considered absolutes for any given person. Individual experiences may vary based on several factors, including:
- Overall health
- Specific fertility concerns
- Quality of eggs and sperm.
These factors should be discussed with an IVF doctor.
Cumulative Success Rates and Additional IVF Cycles
When considering the effectiveness of IVF treatments, it is essential to examine cumulative success rates. Basically, the more times a patient attempts IVF, the higher their chances of having a baby. Regardless of age, the cumulative success rates for IVF almost always increase with additional cycles, whether from frozen embryo transfers from one egg retrieval or from multiple egg retrieval cycles. Understanding the cumulative success rates provides a better perspective on the potential outcomes of multiple IVF treatment cycles.
Multicycle Plans for Increased IVF Success
Many couples may not achieve success with their first IVF cycle. In such cases, purchasing separate treatment cycles each time can be financially challenging. To address this concern, some fertility clinics offer multicycle IVF plans that provide more chances for IVF success at a lower cost per cycle.
Multicycle plans often include a predetermined number of IVF cycles, which can significantly reduce the costs associated with multiple attempts. This option allows families to continue their IVF journey with increased optimism and determination.
Click here to learn about ARC Fertility’s Multicycle IVF Packages.
IVF Success Rates with Donor Eggs
The effectiveness of IVF is influenced by several factors, including the type of treatment, which can include:
- Using an intended parent’s own eggs
- Using donor eggs
- The intended parent’s age, particularly if over 35 years old
When it comes to IVF success rates, older women who use donor eggs generally have higher chances of achieving a successful pregnancy compared to using their own eggs. Donor eggs typically come from younger individuals, offering better chances of successful fertilization and implantation during IVF.
Chances of successfully having a baby significantly increase when utilizing donor eggs, as demonstrated in the figure from the CDC.
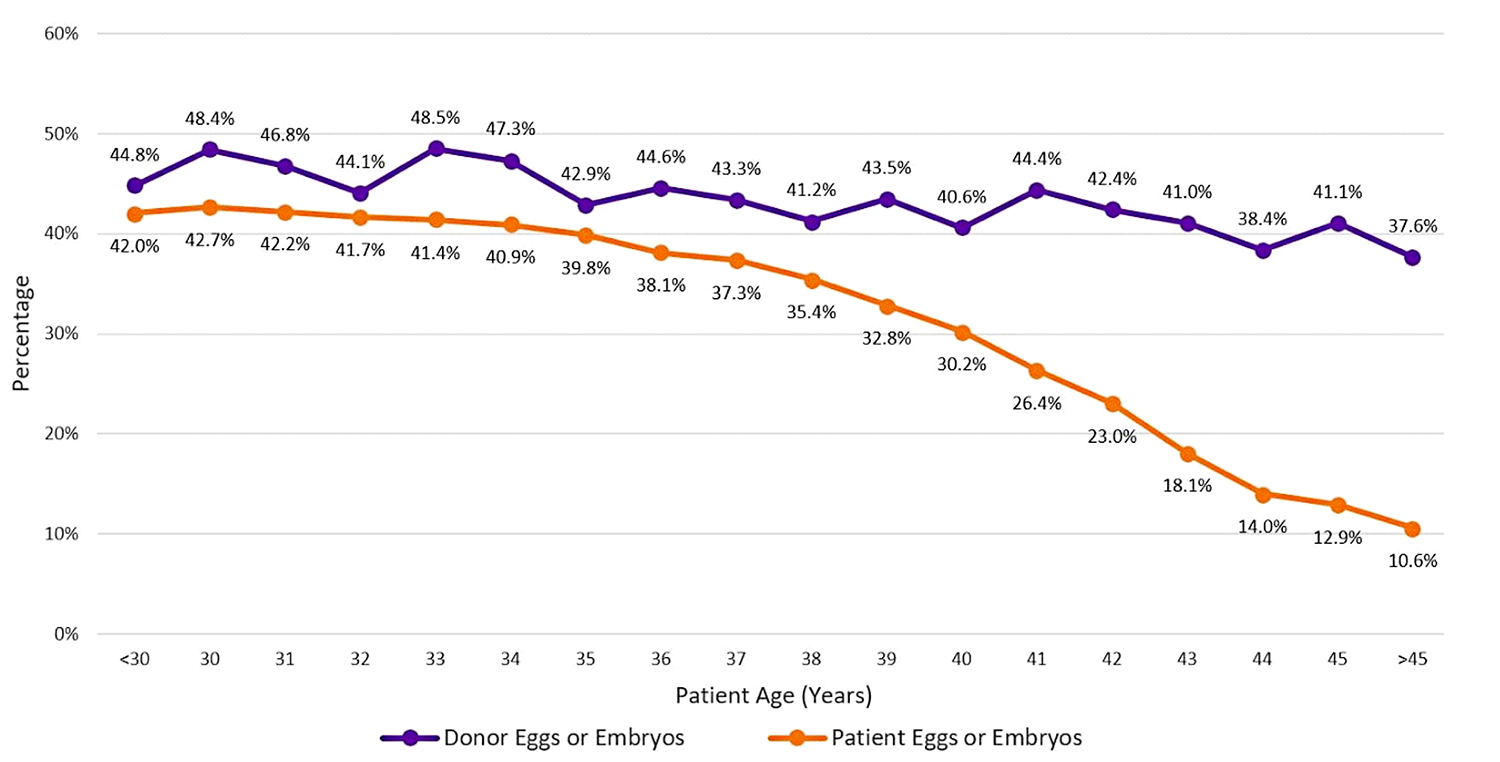
Explaining the chart
This figure shows the percentage of embryo transfer cycles started in 2020 that resulted in live-birth delivery of one or more live infants, by patient age and egg or embryo source. Fresh and frozen eggs or embryos from patients and donors are included. Banking cycles in which all eggs are frozen and not used immediately are excluded.
The percentage of live births resulting from embryo transfer cycles using patient eggs or embryos decreased as the age of the woman increased (range: 42.7% to 10.6%).
In contrast, 41.4% of embryo transfer cycles using donor eggs or embryos resulted in live-birth delivery for women of all ages (range: 37.6%–48.5%). Egg donors are typically in their 20s or early 30s and do not have infertility.
It should be noted that these live birth rates are higher than those in the tables above because they are live births per embryo transfer in the graph and are live births per intended egg retrieval in the tables above. The difference is that some patients, especially older, do not develop enough eggs to undergo egg retrieval, some do not get any eggs at retrieval, some get eggs that are not fertilized, and some with fertilized eggs do not develop embryos that can be transferred. So the live births per embryo transfer include only those women who could successfully go through all those steps to create an embryo good enough for transfer.
Donor Egg Packages
Many fertility clinics offer Donor Egg Packages as IVF treatment options. These packages bundle the use of donor eggs with IVF procedures for families seeking fertility assistance. By offering these bundles, clinics aim to streamline the process and provide a more convenient and cost-effective solution for patients who need donor eggs for successful fertilization and pregnancy.
Learn more about ARC Fertility’s Donor Egg Packages.
Maximizing IVF Success Rates
The following are major factors when it comes to IVF success rates:
- Multiple cycles can significantly enhance the chances of achieving a successful pregnancy. While we cannot control our age, there are certain factors within our control that can influence the outcomes. By focusing on lifestyle choices and overall health, individuals can improve their IVF journey.
- Maintaining a healthy weight and following a balanced diet can contribute to well-being and improve IVF success rates. Avoiding smoking and minimizing caffeine and alcohol intake are additional lifestyle choices that can boost fertility and help produce a successful outcome.
- Individuals 40 years old or older, or with a diminished ovarian reserve, should consider using an egg donor to greatly enhance their chances. Donor eggs offer a higher chance at successful fertilization, implantation, and delivering a healthy baby, particularly when a patient’s own egg quality and quantity may be compromised due to age.
While age maintains a significant impact on IVF success rates, taking control of these modifiable factors can optimize outcomes. By making informed choices and working closely with fertility specialists, many individuals can realize their dream of starting or expanding their family through IVF.
Consult with a Fertility Specialist
To optimize your chances of success with IVF, consult with a fertility specialist who can assess your unique circumstances and develop a treatment plan tailored to your needs. Their expertise will ensure you receive the most appropriate interventions and strategies for maximizing your chances of a successful and healthy birth.
Related Content:
Your Top IVF Questions – Answered!
How is IVF Done, Step by Step?
ARC IVF Success Rate & Cost Calculator
Advantages of Multiple IVF Cycle Treatment Packages
NOTES: References for CDC Data
https://www.cdc.gov/art/reports/2020/summary.html#table

